Recalls disrupt workflows, affect patient confidence, and force orthopaedic practices to re-evaluate how they monitor implant performance. If you’re managing patient populations with recalled devices, your clinical decisions hinge on identifying failure risks before they escalate. Implant failures rarely happen for a single reason, and post-recall screening requires a deeper understanding of mechanical limits, biological responses, and design vulnerabilities. Quality control failures upstream in the manufacturing process add another layer of complexity once the implants are already in patients. The following approach integrates current evidence, material testing standards, and practical insights so that your response strategy is both proactive and adaptive.
Failure screening starts with understanding implant vulnerabilities
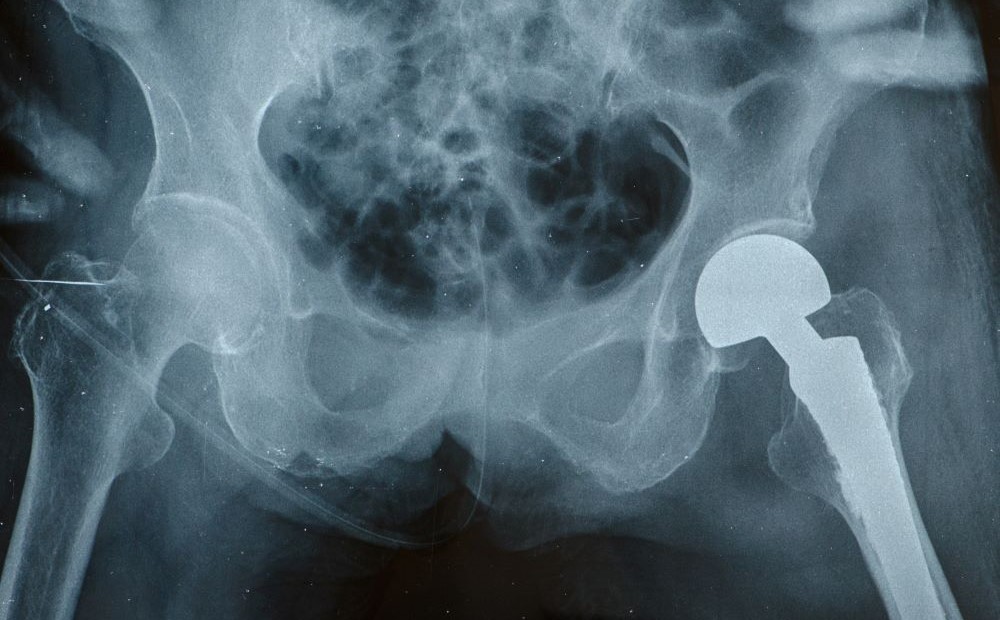
You’ve likely encountered implant failures related to infection, material fatigue, or biomechanical misalignment. Each of these pathways has its own set of markers, but the clinical outcome converges in pain, instability, or loss of function. Common causes include poor bone quality, implant corrosion, and non-union at the fracture site (7). When patients return with persistent discomfort or abnormal imaging, you’re often dealing with progressive deterioration rather than a sudden defect. Failures related to mechanical overload or repetitive microtrauma may remain silent until late in the postoperative course, which complicates surveillance timing.
Identifying patients at risk requires a layered screening approach. Focus first on core risk indicators:
- Surgical history
- Fracture type and location
- Implant material and geometry
- Bone density and patient-specific biomechanics
- Comorbid conditions such as diabetes or smoking history
Then expand to include imaging modalities that detect early signs of implant loosening, wear, or osteolysis. You’ll catch more failures early when you combine symptom tracking with structured follow-up intervals.
Device safety depends on manufacturing quality and validation
Not all recalls originate in the OR. Flaws introduced during the design or manufacturing stages can compromise the device long before you use it. Quality control lapses, whether in material purity, dimensional tolerances, or surface treatments, remain a common cause of systemic implant issues. You need confidence that every device has passed rigorous validation steps, especially fatigue and corrosion resistance.
Proper mechanical validation helps bridge this trust gap. As outlined in “Orthopedic Manufacturing Best Practices,” mechanical testing simulates real-world stresses across a device’s life cycle. Fatigue testing, for instance, replicates long-term cyclic loading to expose points of weakness. If those benchmarks aren’t met, implants are more likely to fail once integrated into biological systems. This is where the manufacturing process needs oversight because precision tools like CNC machines or additive manufacturing systems depend on consistent calibration and strict post-processing standards.
Standardized testing protocols improve predictability in performance
You’ve probably seen variability in implant outcomes even when using the same product line. This variability underscores why standardized testing isn’t optional. The ASTM F565-21 standard, for example, outlines protocols for care and handling of orthopaedic implants and instruments, including sterilization, packaging, and labeling. Following these guidelines is part of risk mitigation, especially when working with vendors or evaluating new implant systems.
The most informative mechanical tests include:
- Tension and compression loading
- Bending resistance
- Fatigue and cyclic durability
- Torsional strength
- Wear performance under simulated joint articulation
When manufacturers follow these protocols consistently, your practice benefits from predictable implant performance across different patient types. More importantly, you gain clarity when assessing whether a failure stems from clinical use or manufacturing inconsistency.
You need a monitoring system that adapts to failure patterns
Post-recall, surveillance becomes your strongest clinical tool. Longitudinal monitoring of patients with recalled implants gives you the chance to detect subclinical failures before they convert into major complications. That monitoring process should include a mix of radiographic evaluations, lab markers when infection is suspected, and structured symptom checklists.
In a retrospective study of implant revision cases, ongoing follow-up revealed patterns that weren’t initially visible on standard imaging. These silent failures often present late, especially in asymptomatic or low-demand patients. That’s why regular follow-up, regardless of symptom presence, matters. Early intervention is more likely when you track patterns across patient subsets.
Even when the device is at fault, you’re not automatically liable. Manufacturing defects typically account for a small percentage of failures and aren’t considered negligence unless there’s a breach in clinical judgment. Still, documenting decision-making steps, patient education, and monitoring plans remains essential.
Post-recall management is an active, continuous process
Managing implant failures after a recall requires more than reactive care. You’re constantly making decisions in an evolving context. These decisions are shaped by implant design, biological response, and patient behavior. The variability of failure mechanisms forces you to think in terms of risk stratification rather than isolated events. Surveillance, mechanical validation, and knowledge of material limits form the foundation of a stable post-recall protocol.
As implant technology advances and new materials enter the market, your role shifts from end-user to clinical gatekeeper. Your ability to evaluate risk, interpret performance data, and act on early signals determines outcomes long before revision becomes necessary. Sustaining that vigilance across clinical, technical, and procedural domains positions your practice to handle recalls not as disruptions but as signals for system improvement.
Sources
A novel concept of an acoustic ultrasound wearable for early detection of implant failure
How To Improve Orthopedic Implant Safety?
Implant Failure in Orthopaedics: Law Does Not Hold the Surgeon Accountable
Orthopedic Implant Testing Guide
Standard Practice for Care and Handling of Orthopedic Implants and Instruments
The Importance of Quality Control in Orthopedic Implant Manufacturing





