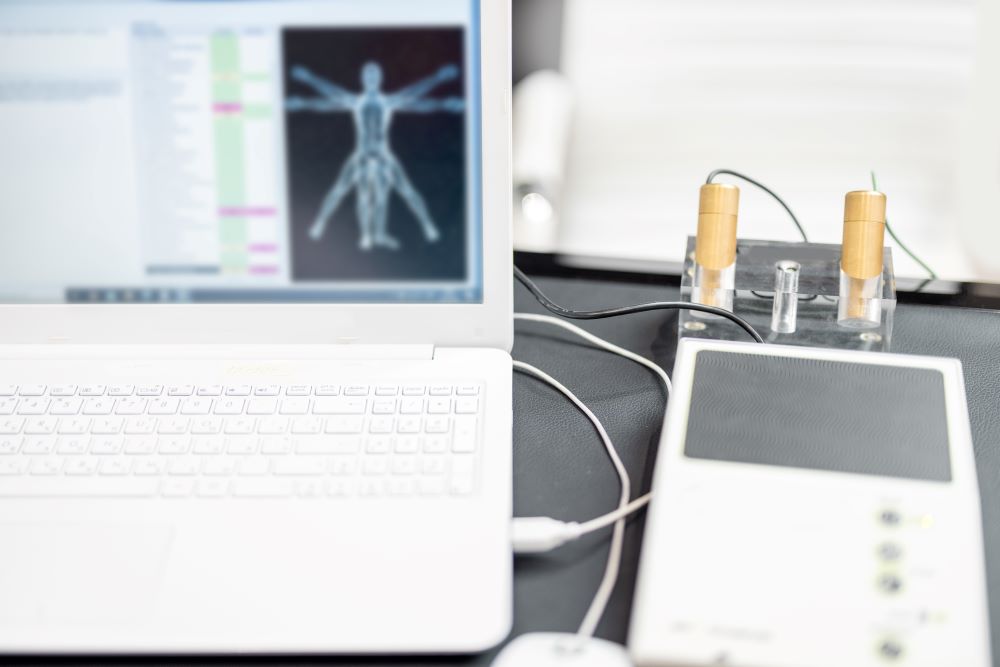
Digital twin (DT) technology has caught the attention of orthopaedic professionals for good reason. The idea is simple on the surface: Create a real-time, digital version of a patient’s musculoskeletal system to simulate what might happen in the clinic, the OR, or during rehab. But what happens when the theory becomes something you can actually use? More tools are becoming available, and many of them aren’t just research concepts anymore.
You’re probably already using some of the raw inputs a digital twin would need — MRI data, motion analysis, gait reports, implant performance. What DTs add is integration. Instead of juggling individual pieces of information, you get a living model that brings them together in one place, structured around a patient’s real anatomy and movement. It doesn’t replace your judgment. It just lets you test it first.
Digital twins build on models you already trust
If you’ve used finite element models or multibody simulations in research or device planning, then you already know what a digital twin is made of. The difference is that DTs are tied to real patients, often updated with sensor data or imaging inputs that evolve over time. For musculoskeletal care, that includes joint contact mechanics, load distribution, muscle force predictions, and range-of-motion analytics.
Here’s how digital twins are already helping in clinical decision-making
In knee osteoarthritis, patient-specific DTs have been used to model how cartilage wear patterns progress under various loading conditions. A clinician can simulate altered gait patterns or brace interventions and project how they might delay joint space loss.
In spine care, models have recreated adolescent scoliosis progression. You can adjust disc stiffness, growth rates, and brace tension in the twin and see what the outcome might look like two years out before making that call in the exam room.
In total knee arthroplasty planning, DTs are being tested to simulate implant alignment strategies. Instead of depending on templated sizing and generic kinematic predictions, you can see what effect different tibial rotations or slopes might have on patellofemoral tracking and flexion stability.
Each example shows the same pattern. You feed in patient-specific data, define possible treatment paths, and let the twin show you what might happen.
Surgical planning becomes more precise and more visual
You’ve likely been through preoperative planning platforms that help estimate implant fit or alignment. A digital twin adds the next layer by letting you test outcomes. You’re evaluating how they interact with soft tissue constraints, contact pressures, and expected ranges of motion.
Some teams are even using DTs during the planning phase to spot complications before they occur. Say you’re working on a patient with a challenging femoral deformity. Before the OR lights turn on, you simulate the plan, notice an impingement risk during mid-flexion, adjust the resection angle in the twin, and proceed with confidence.
Postoperative tracking is starting to loop back into the model
Wearable sensors and rehab apps already gather data on recovery. What’s new is feeding that information back into the twin to see whether recovery is on track. For example, a DT can flag an asymmetrical gait pattern that deviates from expected norms, suggesting delayed muscle recovery or joint stiffness. You get an early signal and a direction to investigate before the patient returns with pain or dysfunction. In some pilot programs, recovery data has already altered rehab timelines and reduced readmission risk.
The roadblocks are real but they’re being tackled
Like any new tool, DTs come with friction. If you’ve tried early systems, you might have seen:
- Long model setup times
- Confusing interfaces
- Gaps in integration with PACS or EMRs
- Limited support for different implant systems or procedural workflows
But improvements are happening fast. Standardization efforts are underway to improve data acquisition consistency and interface design. Some platforms now offer drag-and-drop model inputs or cloud-based simulations that run in minutes, not hours. And more collaborations between orthopaedic teams, engineers, and data scientists are helping align tools with actual clinical workflows.
Digital twins won’t replace your expertise but they might sharpen it
Think of a digital twin as a second set of eyes, not a second opinion. It lets you ask “what if” before a scalpel touches skin. It helps you anticipate outcomes instead of reacting to them. And it gives you a clearer sense of how a specific body, under specific loads, might respond to the choices you’re about to make.
You don’t need to become a modeler or coder to make use of this. What matters is having tools that meet you where you are, whether that’s in the clinic, in the OR, or in the treatment planning room. Whether the technology becomes routine will depend on how easily it fits into your process and how reliably it improves it.
Digital twins are starting to act like real assistants in your workflow. And as they get faster, more intuitive, and better connected to patient outcomes, the question becomes less about whether they’re the future and more about how soon they’ll be your everyday tool.
Sources
Digital twin assisted surgery, concept, opportunities, and challenges
Leveraging digital twins for improved orthopaedic evaluation and treatment
Patient-specific spine digital twins: a computational characterization of the idiopathic scoliosis
The status quo and future prospects of digital twins for healthcare
This article is intended for informational purposes only and does not constitute medical or professional advice. The content reflects emerging research, evolving clinical applications, and expert perspectives in the field of digital twin technology for musculoskeletal care. It is not a substitute for personalized medical evaluation or consultation with a qualified healthcare provider. The use of digital twins—whether in surgical planning, rehabilitation monitoring, or orthopedic decision-making—carries inherent limitations and may vary in effectiveness depending on patient-specific factors, technological platforms, and clinical protocols. Orthopaedic professionals and patients should consult with board-certified specialists to determine the most appropriate, evidence-informed course of action for individual needs. Clinical decisions should always be based on direct medical assessment and professional judgment.





